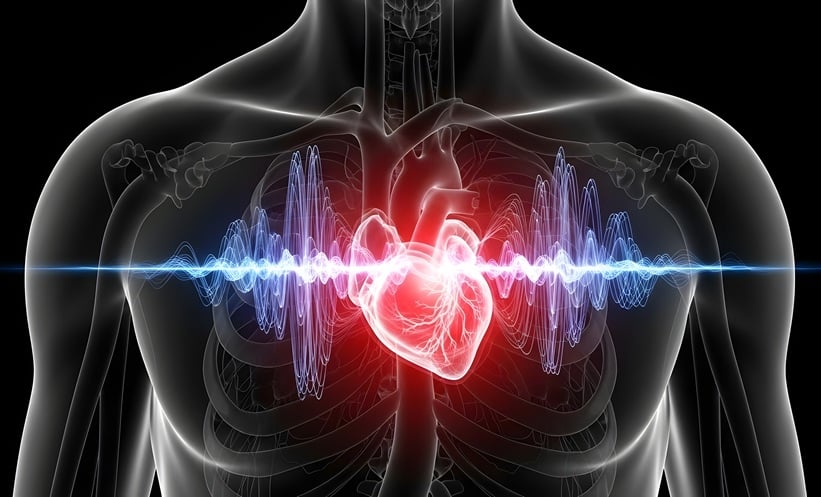
Heart Health Breakthrough: 3D Cardiac Mapping Transforms the Way Arrhythmia Is Detected
Cardiac arrhythmias remain one of the most serious and widespread heart health challenges worldwide, contributing significantly to stroke, heart failure, and sudden cardiac death. For decades, accurately identifying where abnormal heart rhythms originate has required invasive procedures that carry risks and limitations. Now, groundbreaking research suggests a powerful alternative: three-dimensional, non-invasive cardiac mapping that can pinpoint arrhythmia sources with unprecedented accuracy.
Why Arrhythmia Mapping Matters
Arrhythmias occur when the heart’s normal electrical signaling is disrupted, causing irregular, rapid, or dangerously slow heartbeats. Successfully treating these conditions—especially through catheter ablation—depends heavily on one critical factor: precise localisation of the abnormal electrical activity.
If clinicians can’t accurately identify where the faulty signals begin, treatments may be incomplete, less effective, or require repeat procedures. Traditional electrocardiographic imaging techniques usually reconstruct electrical activity only on the heart’s surface, known as the epicardium. While helpful, this surface-level view often fails to detect arrhythmias that originate deeper within the heart muscle, or myocardium.
A Major Leap: Volumetric 3D Cardiac Mapping
The new research introduces a volumetric, non-invasive cardiac mapping approach that goes beyond the heart’s surface and reconstructs electrical activation throughout the entire three-dimensional heart muscle. This represents a fundamental shift from conventional methods.
Using body-surface electrical signals combined with advanced computational modeling and mathematical techniques known as Green’s functions, researchers solved a complex inverse problem. In simple terms, they worked backward from signals detected on the body to accurately reconstruct where electrical activity occurs inside the heart.
Heart Health Breakthrough as 3D Cardiac Mapping delivers sharper accuracy and new hope for safer, non-invasive arrhythmia care
The results were striking.
Dramatically Improved Accuracy
Compared with surface-only mapping approaches, the volumetric 3D method reduced geodesic localisation error by 59.3%. This means the system was far more accurate at identifying the true origin of abnormal electrical signals—a critical improvement for both diagnosis and treatment planning.
Accurate localisation is especially important in complex rhythm disorders, where arrhythmias may arise from deep or unusual regions of the heart that surface mapping simply cannot capture.
Tested in Complex, Real-World Cases
The technique was evaluated using both simulated and real clinical scenarios. Researchers tested it on simulated premature ventricular beats and on four patients with clinically challenging rhythm disorders, including:
-
Ventricular tachycardia
-
Left bundle branch block
-
Wolff–Parkinson–White syndrome
-
Premature ventricular contractions originating from the right ventricular outflow tract
In every patient case, the reconstructed activation patterns closely matched the clinical diagnoses. This consistency supports the method’s real-world relevance and potential for translation into clinical practice.
Why Non-Invasive Matters
Currently, the gold standard for detailed arrhythmia mapping involves invasive catheter-based procedures. While effective, these techniques come with risks such as bleeding, infection, longer recovery times, and higher costs. They also require highly specialized facilities and expertise, limiting accessibility in many parts of the world.
By contrast, non-invasive volumetric cardiac mapping could:
-
Reduce procedural risk
-
Improve patient comfort
-
Expand access to advanced arrhythmia diagnostics
-
Lower healthcare costs
-
Enable better pre-procedural planning
Avoiding invasive mapping could be especially valuable for patients who are elderly, medically fragile, or unsuitable for catheter-based diagnostics.
Implications for Treatment and Planning
The findings suggest several major clinical benefits. More accurate 3D mapping could significantly improve pre-procedural planning for catheter ablation, helping physicians target abnormal tissue more precisely and potentially reducing the need for repeat procedures.
In addition, the technology may refine candidate selection for cardiac resynchronisation therapy, a treatment used in certain heart failure patients to restore coordinated heart contractions. By better understanding the heart’s electrical activation patterns, clinicians could tailor therapies more effectively to individual patients.
Beyond Arrhythmias: Broader Applications
Performance of the new mapping approach was also assessed using an open-source dataset related to myocardial infarction estimation. This suggests the technology may have applications beyond arrhythmia detection, potentially aiding in the assessment of heart damage after a heart attack and other structural or electrical heart disorders.
Important Limitations to Consider
While the results are highly promising, researchers caution that the study involved a relatively small number of patient cases. Larger clinical trials will be necessary to validate the findings across diverse populations and a wider range of arrhythmias.
Additionally, while improved mapping accuracy is a crucial step, future studies will need to determine whether integrating this technology into routine clinical workflows leads to better long-term outcomes, such as reduced recurrence of arrhythmias, fewer complications, and improved survival.
The Future of Cardiac Care
Despite these limitations, the study marks an important milestone in heart rhythm care. By extending non-invasive cardiac mapping from the heart’s surface into the full three-dimensional myocardium, researchers have opened the door to safer, more accurate, and more accessible arrhythmia diagnosis.
Read Also : Aryna Sabalenka Survives 1 Scary Test, Powers Through a Ruthless Australian Open Start
If future studies confirm these findings, volumetric 3D cardiac mapping could fundamentally change how clinicians detect, plan, and treat complex heart rhythm disorders—shifting care away from invasive diagnostics and toward smarter, patient-friendly technologies.
In a field where precision can mean the difference between life and death, this game-changing heart breakthrough may signal a new era in arrhythmia detection and treatment.